 As the instructor zipped open the bag containing the body of our 74 year old female donor, my eyes took in the sight of feet, legs, hips, abdomen, arms, shoulders, head all softly and quietly at rest. And yet, something was quite obviously out of place. Nothing screams implant like a 74 year old cadaver with perky breasts.
As the instructor zipped open the bag containing the body of our 74 year old female donor, my eyes took in the sight of feet, legs, hips, abdomen, arms, shoulders, head all softly and quietly at rest. And yet, something was quite obviously out of place. Nothing screams implant like a 74 year old cadaver with perky breasts.
Surgical procedures are described and illustrated in detail in this post. Please be advised if you are sensitive to the subject matter.
Although we didn’t know exactly the year in which Rose acquired these augmentations or why she opted for enhancement, there were many indicators which hinted to the possibility that she’d received them possibly in her mid 50’s. It was also possible she received them for elective cosmetic reasons.
The type of scar was a crescent shape under each breast. This was a common way to implant about 20 years ago. Today, preferred implant routes include through the nipple, through the axilla (armpit), or via the umbilicus (belly button). Also, the scar was quite mature and well blended into the body.
The shape of the implant was round and appeared to be of the older, more volatile silicon solution. This type of implant was discontinued due to the possibility of rupture and the silicon leaking into the body. Newer silicon implants are more gel-like & do not leak if they are severed and more recently they have even developed a more teardrop shaped implant.
The location of these implants was directly under the skin. Most implants these days are inserted under the pectoral muscle and not the skin due to the skin’s tendency to loose tensile strength over time which may result in the implant location sagging.
We can only speculate that Rose may have acquired these implants as an elective enhancement of some kind. The only thing present between the skin and pectoral muscle was the implant. We rejected the possibility of cancer, as there was no evidence of radiation or chemotherapy.
Although the instructor had plenty to show us in detail around the neck and knee, I’m somewhat uncomfortable to admit to find I was obsessed with this 74 year old woman’s breasts. I just couldn’t wait to get my hands on them (yes, you can laugh at that)! Finally the instructor asked who would like to remove the left breast implant so the class could examine it. I was practically standing in his surgical smock pocket before he finished uttering the invitation. Thank God he gave me the scalpel. I shudder to think what I’d have done if he’d have handed it to someone else. Containing my jack russell terrier type excitement, I listened carefully to his instruction on how to use the scalpel, where he wanted me to cut and how to proceed. I took a big breath and began a crescent style cut that skirted the original incision so the class could observe the underlying adhesion of the original surgery.
As I lifted the flap I had created from my incision, a round implant, encased in a facial compartment adhered to the posterior side of the breast. I worked gently to release this from the skin and once it was free, the class took a moment to examine it.
The myofacial covering appeared quite sturdy, relatively unyielding, & slightly oval shaped with a flatter bottom side that had been next to the pectoral wall. The entire structure, covering and implant, weighed about 1-2 pounds and seemed to be harder than a natural breast. I had seen implants as well at cosmetic surgery open houses that were significantly softer as well as not nearly this compact in shape. They tended to spread more than this.
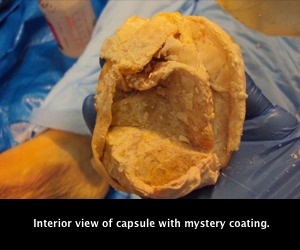
 The instructor requested I continue my investigation and suggested I attempt to free the implant from the myofacial compartment. Very carefully I attempted to pierce the covering without rupturing the implant. The first few swipes revealed the sac was made up of two distinct substances styles. The most superficial was a fibrous yet flexible tissue. The inner layer however seemed to be lined with something. It became evident quite quickly that the implant itself was not adhered to in any way. It was simply cocooned in this odd sac. Opening a large enough window to free the implant, the class was shocked to discover this myofacial cocoon to be lined entirely with a calcium style substance. It was almost as if someone had painted the entire interior of the compartment with a thick milk paint. As I turned the capsule inside out, the substance on the inside walls cracked and revealed it to be a calcium-like lining which flaked easily from the walls of the myofacial tissue.
The instructor requested I continue my investigation and suggested I attempt to free the implant from the myofacial compartment. Very carefully I attempted to pierce the covering without rupturing the implant. The first few swipes revealed the sac was made up of two distinct substances styles. The most superficial was a fibrous yet flexible tissue. The inner layer however seemed to be lined with something. It became evident quite quickly that the implant itself was not adhered to in any way. It was simply cocooned in this odd sac. Opening a large enough window to free the implant, the class was shocked to discover this myofacial cocoon to be lined entirely with a calcium style substance. It was almost as if someone had painted the entire interior of the compartment with a thick milk paint. As I turned the capsule inside out, the substance on the inside walls cracked and revealed it to be a calcium-like lining which flaked easily from the walls of the myofacial tissue.
 Suddenly the class was a whirl of questions & suggestions as to what and why. We broke for lunch discussing the possibilities. Was the body attempting to reject the implant? Is this why women complain of implants feeling hard after several years? There was no rupture to the implant so the contents of the implant were not in question regarding contaminating the compartment. Would women want these if they knew this would happen later in life? Did the doctor know this kind of thing happened?
Suddenly the class was a whirl of questions & suggestions as to what and why. We broke for lunch discussing the possibilities. Was the body attempting to reject the implant? Is this why women complain of implants feeling hard after several years? There was no rupture to the implant so the contents of the implant were not in question regarding contaminating the compartment. Would women want these if they knew this would happen later in life? Did the doctor know this kind of thing happened?
By the time the lunch break concluded my obsession regarding the implants had only increased. Over lunch, one of my colleagues had suggested that maybe the pacemaker might have influenced this calcium style lining in some way. In addition, one of the anatomy lab owners said that the implants he had removed in other dissections never had calcium build up inside that myofacial compartment. I had to see what the other implant looked like. I was most pleased when the instructor suggested I remove the other breast and free the other implant while he and the teaching assistant opened windows in the rib cage. Overcoming that odd sensation that accompanies carrying a disembodied breast across a room, I settled at the other table next to another student who was dissecting the lower leg and happily continued my investigation.
 This implant freed quite like the other one had from the skin. The look and feel of the encapsulated implant was very similar to it’s left sided partner & yet, something was different. With the first swipe of the scalpel on the surface, the reason became clear. Almost immediately, I had nicked the implant. (This was the indicator as well that this was the older silicon model as the contents leaked but didn’t spill out through the hole I’d made in the implant.) This cocoon was unlike its predecessor in that it wasn’t as thick. Working even more carefully than before, I opened a window just large enough to slip the implant out. The remaining sac was fibrous and flexible just like the first one except this one had no calcium built up on the inside! When I turned the sac inside out, it was perfectly smooth and flexible. You could even see the seams of the implant like a fingerprint on this inner wall!!!
This implant freed quite like the other one had from the skin. The look and feel of the encapsulated implant was very similar to it’s left sided partner & yet, something was different. With the first swipe of the scalpel on the surface, the reason became clear. Almost immediately, I had nicked the implant. (This was the indicator as well that this was the older silicon model as the contents leaked but didn’t spill out through the hole I’d made in the implant.) This cocoon was unlike its predecessor in that it wasn’t as thick. Working even more carefully than before, I opened a window just large enough to slip the implant out. The remaining sac was fibrous and flexible just like the first one except this one had no calcium built up on the inside! When I turned the sac inside out, it was perfectly smooth and flexible. You could even see the seams of the implant like a fingerprint on this inner wall!!!
If I didn’t have enough questions before, I now had a treasure trove of them. Was it indeed the electrical current that had caused the calcium build up? Was it a lack of circulation to the left breast? Even more so, could integrated manual therapy have helped prevent the calcium build up? Also re-occurring was the question of are the breast implants women complain about getting hard actually building this calcium lining or is it just a result of this tight myofacial compartment preventing the implant from yielding and spreading under pressure.
I got my answers to these questions a few weeks later after I booked a consultation with a local plastic surgeon. As it is difficult to get an appointment merely to ask questions about a dissection class, I went in under the pretense of wanting breast implants of my own but had concerns based on a recent dissection class I had participated in. I was fascinated to get explanations to my findings.
It was indeed natural to find the implant encapsulated by tissue. This is the body’s natural response to a foreign substance it can’t remove. We also found a similar membrane around the pacemaker as well as the wire running to the heart. The hip implant, since it was only a couple weeks old, showed no evidence yet of such a membrane.
Where the breast was concerned, however, Rose was most likely suffering from a case of capsular contracture. Wikipedia defines as such:
- “Capsular contracture is an abnormal response of the immune system to foreign materials in the human body. Medically, it occurs mostly in context of the complications from breast implants and artificial joint prosthetics.”
In the case of the breast implant, collagen fiber capsule tightens around the breast implant and squeezes causing pain and may even distortion the appearance of the breast implant in some cases. This was most certainly the case where Rose was concerned. Although I can’t speak to the pain she might have experienced from it, the distortion was evident even as she was lying on the table. Once the implants were removed, the tightness of the myofascial compartments of both implants was quite evident as well.
According to the surgeon I spoke with, capsular contracture may have occurred as a result of a bacterial infection. “Back in the day,” as she put it, breast implant surgeries were often done in the doctor’s office and not in a surgical room. The possibility of infection was greater in these incidents. As the implants were clearly older, as she verified looking at the dissections photos I provided, this was a likely scenario for Rose. An additional contributing factor to the capsular contracture was most likely the fact that Rose was a smoker as that is another suspected cause of this condition.
 Although both breast capsules indicated capsular contracture condition, only one had the calcium-like lining. This was another indicator, according to the surgeon, that this was most likely an older procedure. One method of treating contractures was the injection of certain steroids such as Kenalog. This was one of the methods doctors would use to combat capsular contracture and would leave such a residue within the capsule. Why she only had one breast treated and not the other is unknown but it was indeed interesting to note the differences.
Although both breast capsules indicated capsular contracture condition, only one had the calcium-like lining. This was another indicator, according to the surgeon, that this was most likely an older procedure. One method of treating contractures was the injection of certain steroids such as Kenalog. This was one of the methods doctors would use to combat capsular contracture and would leave such a residue within the capsule. Why she only had one breast treated and not the other is unknown but it was indeed interesting to note the differences.
The implants demonstrated beautifully one risk that exists for the person who receives implants. Tissue appearance, relationships to other structures in the body, as well as condition of Rose overall can help provide clues to possible preventative avenues in manual treatment options. The surgeon I interviewed stated that, although the procedures are indeed better today than when Rose had her implants, capsular contracture does indeed still exist and occurs on occasion. According to Wikipedia, all prosthetic implants, not just breasts, may experience this phenomenon . Germ contamination, placement of the implant above the muscle (still and option for breast implantation), infections, seromas, or hematoma are all suspected for contributing to capsular contracture. Smoking as well as it decreases oxygen levels in the blood which can lead to delayed healing.
Thinking back on the findings, one wonders, if Rose had received integrated manual therapy pre and post surgery, would capsular contracture ever had occurred? Now that we have a better understanding as to what could potentially go awry with implants, the answer to this question hopefully will be able to be demonstrated in the future.


0 Comments